
Spondylolisthesis is a term that derives from 2 words; namely spondylo which means vertebra (a segment of back bone / spine) and listhesis which means slippage. It refers to a condition where a vertebra slips forward in relation to the vertebra below it. It more commonly happens at the level L4/L5 and L5/S1 of lumbar spine than other levels of spine.

Symptoms of Spondylolisthesis
This condition causes mechanical back pain to the patient, especially after exercise. In cases of advanced slippage, the patient would compensate with increased lumbar lordosis (sway back) and extension of the hips causing hamstrings tightness. In some cases, when the nerve is compressed by the slippage, it causes radicular pain (buttock to leg shooting pain, sciatica), weakness and numbness to one or both legs. In severe cases, it can also cause urine and bowel incontinence (loss of control). Occasionally, people with spondylolisthesis have no symptoms and only find out the problem incidentally.

Causes and Type of Spondylolisthesis
There are several main causes of spondylolisthesis and they are classified as such:
Type I: Congenital / Dysplastic.
This happens when there is a birth defect at the articular processes of the vertebra. It usually happens at the L5/S1.
Type II: Isthmic.
In this type of listhesis, there is a defect at the pars interarticularis. It is the commonest type among all. It can be further divided into:
Type IIA: Stress fracture due to repetitive micro-fractures to the pars. It is also known as spondylolysis. It commonly occurs in gymnasts and divers.
Type IIB: Elongation of the pars interarticularis as a result of repeated injuries and healings to the pars.
Type IIC: Traumatic pars fracture due to high impact injury such as car accident and fall from height.
Type III: Degenerative.
The spine degenerates as the aging process progresses, leading to wear and tear of the intervertebral disc, the facet joints and the surrounding ligaments. Eventually the vertebra body slips forward as the joints and ligaments can no longer holding it in place. Degenerative spondylolisthesis commonly happens at the level of L4/L5.
Type IV: Traumatic.
Fracture to other parts of the vertebra, other than the pars interarticularis (Type IIC). For instance, pedicle fractures, facet fractures, etc.
Type V: Pathological.
Infection and tumour of the spine may sometimes cause spondylolisthesis because of the destruction the vertebra leading to instability.
Type VI: Iatrogenic.
If a spine surgery causes weakening of the pars interarticularis and subsequently slippage of the vertebra, it is termed as iatrogenic spondylolisthesis.
Severity of Spondylolisthesis
The severity of spondylolisthesis can be graded according the percentage of slippage.
| Grade I | Less than 25% of slippage |
| Grade II | 25-50% |
| Grade III | 50-75% |
| Grade IV | 75-100% |
| Grade V | More than 100% of slippage |
Grade I and II are considered low-grade spondylolisthesis, whereas the grade III and IV are high-grade. Grade V is when the vertebral body completely fallen off from the vertebra below it. Grade V is also known as spondyloptosis.
Diagnosis of Spondylolisthesis
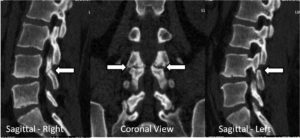
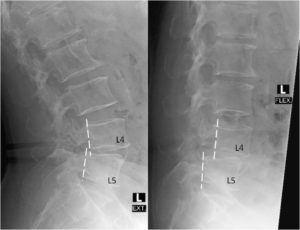
Plain radiograph (X-ray) is the simplest way to diagnose spondylolisthesis. From the lateral (side) standing X-rays, slippage of the vertebra can be clearly seen. X-rays may also giving clue of the underlying causes. Pars interarticularis defect or fracture is best seen in an oblique X-ray (Scotty-dog view). If there is any defect or fracture, the Scotty-dog’s neck would appear broken. In degenerative spondylolisthesis, there will be wear and tear changes to vertebral body, facet joints and disc height but the pars interarticularis remain intact.

In order to examine the stability of the slippage, the patient will be asked to perform 2 additional X-rays in flexion (bending forward) and extension (bending backward). If the slippage changes excessively in these two X-rays, the spondylolisthesis is deemed unstable.
MRI of the spine is required to assess the extent of nerve compression, especially when there are symptoms like radicular pain, weakness, numbness or bowel / urine incontinence.
CT scan of the spine is often necessary to assess the detailed anatomic picture of the vertebra, especially for bony abnormalities.
Treatment of Spondylolisthesis
Most of the patients can be treated non-operatively. The treatment modalities include
- Activity modification and restriction
- Physical therapy to relieve the pain and to strengthen the core muscles of the back
- NSAIDs for pain relief
- Neuropathic pain killer like gabapentin and pregabalin, if there is radicular pain to the leg(s)
- Epidural steroid injections
Surgery is indicated if
- the non-operative treatments fail
- severe intractable back pain
- progressive neurological deficit (worsening of weakness and numbness)
- cauda equine syndrome (neurological deficit with loss of urine and bowel control).
Type of surgery includes:
- Lumbar Decompression and Fusion
Fusion surgery is indicated when the spondylolisthesis is unstable leading to mechanical back pain. Instrumented fusion (using pedicle screw and rod system) has better fusion rate than the non-instrumented fusion. Interbody fusion (bone graft in between the 2 vertebral body anteriorly) has better fusion rate than the posterolateral fusion (bone graft in between the 2 transverse processes and lateral part of facet joints).
There are various way of performing interbody fusion; namely posterior lumbar interbody fusion (PLIF), transforaminal interbody fusion (TLIF), lateral interbody fusion like DLIF, XLIF and OLIF, and anterior interbody fusion (ALIF). Lateral interbody fusion methods are mainly minimally invasive surgeries. TLIF can be performed both conventional open method and minimally invasive method (MIS-TLIF).
- Lumbar Decompression Alone
If the spondylolisthesis is stable in flexion / extension X-rays, decompression surgery is suffice. It usually happens in low grade (grade I, rarely grade II) degenerative spondylolisthesis. The main symptom is usually neurogenic claudication, similar to lumbar spinal stenosis. The spinal segment is stabilized through formation of osteophytes surrounding the vertebrae and enlargement of facet joints (hyperthrophy).


